Chronic Achilles tendonitis – What it means and how to treat it
- Maryke Louw

- Mar 10, 2025
- 9 min read
Updated: Mar 24, 2025
We regularly receive emails from people who’ve been stuck with Achilles pain for more than a year, often several years, asking “Is there any hope of recovery?” The answer is “Yes, absolutely.”
In this article, I’ll explain what chronic Achilles tendonitis means for how severe your injury is and what the chances of recovery are. I’ll also explain what causes it and what treatment we find works best.
Remember, if you need help with an Achilles injury, you're welcome to consult one of our team via video call.

In this article:
We've also made a video about this:
Is it “chronic Achilles tendonitis” or “Achilles tendinopathy”?
In medical jargon, anything with “-itis” at the end means that there’s lots of inflammation involved. In the early or acute stages of an Achilles tendon injury, there is sometimes inflammation, so “tendonitis” is the correct term for that.
However, if the injury has been going on for a long time, there is usually no or very little inflammation, and then “tendinopathy” is more correct.
We’ll mostly use “tendonitis” in this article because that is how most people refer to it, no matter for how long it’s been going on.
Does chronic Achilles tendonitis mean it’s a bad injury?
No. The intensity of your pain and for how long it’s been there do not tell you anything about the severity of your Achilles tendonitis. I realise this sounds counterintuitive, but here’s why.
In medicine, any injury that’s been there for longer than three months is classed as chronic, regardless of how severe it is.
We used to think that pain intensity and how long it sticks around for are directly linked to injury; so, if you have pain, it must mean that you’re injured, and the worse your pain is or the longer it remains, the worse your injury is. However, due to advances in medical scanning and research, we now know that this is not how it works.

For example, researchers recently looked at a group of 145 people diagnosed with Achilles tendinopathy to investigate the relationship between pain and tendon health. They were interested to see how these people’s pain related to their level of function and the severity of the tendinopathy or tendonitis they saw on scans.
They found that the people who reported the highest level of pain and worst function actually had tendons with the same amount of tissue damage as the tendons of those who reported the best function (were able to continue with their sport and other activities) and lowest pain.
And of specific interest to this discussion: The researchers found that how long these people had had their tendonitis symptoms for did not impact the results – chronic Achilles tendonitis did not equate to more severe tendon injuries and did not explain the intensity of the pain.
💡 So, just because your Achilles tendonitis has become chronic or is very painful does not mean it is a very bad case.
Is chronic Achilles tendonitis permanent?
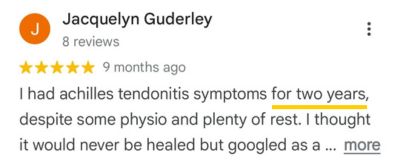
No, it doesn’t have to be. Quite often, our patients have had their symptoms for a year or more before they consulted us, and they still recover, as you can see from the reviews below.
Treating chronic Achilles tendonitis is not complicated, but it does require patience.
I’ll explain exactly how we approach it a bit further down, but first you must understand what causes chronic Achilles pain. Treatment only works if you tailor it to address the most likely reasons why your pain is sticking around.
Top 3 causes of chronic Achilles tendonitis
There are three main causes we’ve identified in the people who consult us with chronic Achilles tendonitis. With some patients it’s only one of these, while others have a combination of these three that needs addressing. And of course, for others it might be something totally different.
1. Doing too much rehab or other activities
When your tendon is injured, it has a limit to how much work it can do in a day. This is not always directly linked to its strength – it may be that your tendon is actually very strong, but it is super sensitive, and if you load it more than a certain threshold, it triggers the pain.

For Achilles pain to settle, you have to adjust your activities to a level that your tendon is currently able to and happy to tolerate. Common mistakes we see people make include:
Doing their rehab too often – your tendon requires some time after exercise to rebuild and strengthen.
Doing exercise in positions that irritate the tendon – this is especially true of tendons that are sensitive to being stretched or compressed over the heel bone.
Using too heavy weights – you might be able to lift it (have the strength), but if your tendon is too sensitive, the pain will be triggered by that weight.
Doing too many or too much of different activities that work the tendon on the same day or week, e.g. walking, running, and rehab.
💡 How much and the type of activities and rehab a tendon can tolerate is different for everyone. This is why it is so important for us to really get to grips with all the relevant aspects of a patient’s life, injury-history, and symptom response.
2. Not doing enough activity or rehab
When you’re in pain, it’s tempting to want to rest the painful area to allow it to calm down. And, yes, rest forms a part of the initial treatment for Achilles tendonitis and it is something we sometimes prescribe.
👉 However, if you rest and protect it too much or for too long, it can actually lead to chronic Achilles pain.
In some cases of Achilles tendonitis, your tendon might lose some strength, which means that it no longer has the capacity to cope with your normal activities (like walking to the shop).

If you rest your injured Achilles for too long or don’t do the correct exercises to restore its lost strength and endurance, it can cause it to lose more strength (like you lose fitness when you stop going to the gym and just lie on the couch for several months).
This reduced strength then means that it can tolerate less walking, running, jumping, etc. before the pain gets triggered.
However, it’s not just a loss of strength that is at play here. There is evidence that if you overprotect an injury, it causes the pain system to become hypersensitised (causing more pain than it should). I explain how this works in the next section.
💡 “Relative rest” is a much better option than complete rest. With relative rest you adjust and adapt the activities that cause pain so that you can remain as active as possible. And you start with simple, very easy exercises and slowly make them more challenging as the tendon is able to tolerate more.
3. Dialled up pain system
As mentioned above, pain is not directly linked to how severe the injury is. Through research we now understand that the level of pain we experience is dialled up or down by our subconscious brains.
It’s the subconscious brain that’s in charge of assessing all the messages it receives from different areas of the body. The idea is that it should only create pain when it thinks you have something in an area of the body that might cause tissue damage or be dangerous to you.
👉 However, it doesn’t just use the signals from your tissues to decide the level of danger. It also considers the impact this injury might have on things like your finances, mental health, social life, and work. For instance, your subconscious might dial your pain level up if it feels an injury might cause you to lose your job.

Do note, this is the subconscious brain we’re talking about – you don’t have any direct control over it with your conscious brain. But there are ways you can get it to stop being so super vigilant and dial the pain down.
Here are examples of things that can cause a pain system to be too sensitive:
Having had pain for more than three months – this “trains” the body to trigger the pain system more efficiently.
Overprotecting your injury.
Fear of making things worse or of what this might mean for your finances, social life, etc.
Chronic stress (this can be work or general life related).
Trying to ignore your pain and push through it – the more you trigger it above a certain level, the more easily it gets triggered.
Certain beliefs or things you tell yourself, e.g. “I will never get better” or “I will definitely need surgery because so-and-so had surgery.”
If you’re a “strong” person who just gets on with things, talking about thoughts and feelings may irritate you and you might think it doesn’t apply to you – I’m the same.
But it’s worth noting that these things are not stuff that just happens in your head. It triggers the body to create physical pathways in the brain and at tissue level that cause the pain system to become “too good” at creating pain. We explain chronic pain in detail here.
💡 A hypersensitised pain system can be brought back to normal through a combination of careful load management (adjusting activities to not exceed specific pain levels) and working on your beliefs, fear, stress, etc. (if needed). These can include simple techniques like positive self-talk, but seeing a sports psychologist or pain psychologist can be very useful in some cases.
How we treat chronic Achilles tendonitis
We've had good success helping people recover from chronic Achilles injuries, but it's important to understand that we don't do anything special or use “weird” techniques you’ve never heard of.
While our approach is not complicated, it’s not a copy-and-paste, one-size-fits-all approach.
1️⃣ We get results where others don’t because we take the time to really discuss and understand our patients' situations and carefully design their rehab plans around them.
2️⃣ We also stay on top of the latest research so that we can look at a person’s situation through an evidence-based lens and let it guide our treatment choices.
Like I mentioned earlier, we often find that the people who consult us have been doing too much rehab, the wrong type of rehab, or that their rehab is fine but how they are ramping up activity needs adjusting. Sometimes, other factors in their lives are also contributing.

We use the information from our assessment to design a starter treatment plan (which may or may not include exercises, depending on what is needed) that we test.
This plan is usually quite simple to start with and is adjusted after the first follow-up consultation, based on the patient’s feedback on how the plan has been working for them.
So, what a patient can expect from our video consultations is:
A thorough conversation and some test movements in the first session.
They'll then get a starter plan that we need them to test for a week or two to see how their body reacts. Tendons need time, and the effect is cumulative; we won’t be able to tell after just one or two days.
The plan might include things like rest, adjustments to shoes, adjustments to daily life or sport, rehab exercises, exercises for other areas of the body, and referrals for other treatments, e.g. shockwave. Every patient’s plan looks different.
We then gather feedback during follow-up consultations and adjust their plans over time.
The plan we start a person on may not look impressive or include things they've never done before; what matters is how it is structured and how it fits with what else they are doing.
We might also suggest they consult a pain psychologist if there are indications that their subconscious brain might be dialling up the pain, and the basic mind techniques aren’t working.
💡 In summary – You don’t need to treat chronic Achilles tendonitis with anything special, but you must make sure the plan suits the individual. What works for one person is likely to need adjustments for the next.
You can find a detailed discussion of the best evidence-based treatments for Achilles tendonitis here and examples of how rehab exercises should be adapted here.
How we can help
Need help with your Achilles injury? You’re welcome to consult one of the team at TMA online via video call for an assessment of your injury and a tailored treatment plan.
We're all UK Chartered Physiotherapists with Master’s Degrees related to Sports & Exercise Medicine or at least 10 years' experience in the field. All of us have a wealth of experience working with athletes across a broad variety of sports and ranging from recreationally active people to professional athletes. You can meet the team here.

About the Author
Maryke Louw is a chartered physiotherapist with more than 20 years' experience and a Master’s Degree in Sports Injury Management. Follow her on LinkedIn and ResearchGate.